Patient Education
Biliary Tract Disorders
Gallstones and Gallstone Disease
Gallstones are stone-like formations that develop in the gallbladder or the bile ducts that connect to the small intestine. They are made up of cholesterol, bile pigment, or both. The most common type of gallstone in the U.S. is cholesterol.
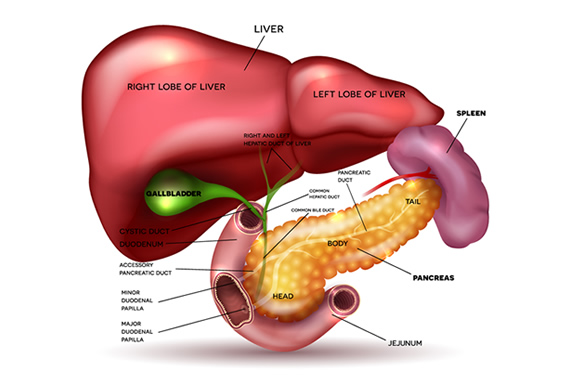
Your gallbladder is a small organ just under your liver on the right side of your body. The gallbladder’s function is to store and dispense a digestive fluid called bile. Bile is important because it helps your body break down the fat in the foods you eat, making it easier to absorb the vitamins and nutrients.
The smallest gallstones are the size of a grain of sand. The largest gallstones can be the size of a golf ball. People with gallstones may not require treatment if they are not causing symptoms. If the gallstones are causing pain or blockages, it may require medication, endoscopy, or complete removal of the gallbladder through surgery.
Gallstones – Symptoms
Many people with gallstones will not have symptoms and won’t require treatment. Sometimes a gallstone may block the flow of bile from the gallbladder, through the bile ducts, or even the pancreatic duct. If a gallstone causes a blockage by lodging in a duct, symptoms can include:
- Pain in the upper right side of your abdomen that starts suddenly and worsens quickly
- Pain in the upper center of your abdomen just below the breastbone that starts suddenly and worsens quickly
- Pain in the right shoulder or between your shoulder blades
- Nausea, vomiting, and sweating
- Jaundice (yellowing of the skin)
Pain can last a few minutes to a couple of hours.
You should seek immediate care if you have the following symptoms that may suggest a more serious problem:
- Pain in your abdomen so intense you can’t find a comfortable position or sit still
- Jaundice (when your skin or the whites of your eyes turn yellow)
- High fever with chills
Diagnosing Gallstones & Gallstone Disease
If gallstones are suspected because of the duration, location, and character of the pain, your doctor may recommend the following tests:
- Ultrasound – An ultrasound allows your doctor to view the gallbladder and associated ducts. Ultrasounds are safe, painless, and are a way of looking at internal organs using sound waves. This is the most common method of diagnosing gallstones.
- Endoscopic ultrasound (EUS) – A small, flexible tube with an ultrasound device is inserted through your mouth and into your digestive tract. This type of ultrasound can find small stones that may have been missed in a typical ultrasound.
- Blood Tests – Blood tests can reveal abnormalities caused by gallstones including jaundice, pancreatitis, or an infection. Higher liver values may be present with gallstones.
- CT Scan – CT Scans are helpful for diagnosing liver and pancreatic cancers. It’s possible to find gallstones using a CT scan, but not as effective as an ultrasound. It may be used to assess the severity of pancreatitis, which can be caused by gallstones.
- ERCP – ERCP stands for Endoscopic Retrograde Cholangiopancreatography. In this test, a doctor inserts a small flexible tube with a camera on the end through your mouth and into your digestive system. A special dye is used to make the bile ducts stand out. If there are gallstones present in the bile ducts, they can be removed at the same time.
- MRCP – MRCP stands for Magnetic Resonance Cholangiopancreatography. This test uses MRI (Magnetic Resonance Imaging) to create images of the bile ducts and pancreatic ducts. It is non-invasive and does not require an endoscopy. If abnormalities are found, ERCP or surgery may be recommended.
Gallstones – Treatment
Treatment is typically not necessary for people who don’t have symptoms. Your doctor will help you decide if gallstone treatment is necessary based on your symptoms and test results.
Even without treatment, it’s important to monitor for symptoms of gallstone complications, including pain in the upper right abdomen. If you have symptoms in the future, you may require treatment.
Gallstone Treatment Options:
- Surgical Removal of Gallbladder: When your gallbladder is removed, it’s called a cholecystectomy. Your doctor may recommend complete removal of the gallbladder because gallstones often recur. You do not need your gallbladder to live and removal doesn’t affect digestion. Instead of bile being stored in your gallbladder, it will flow directly from your liver to the small intestine. Following the surgery, you may need to go to the bathroom more frequently, and your stools may be softer temporarily.
- Endoscopic retrograde cholangiopancreatography (ERCP): If gallstones are obstructing the main bile duct, an ERCP may be an option. This type of endoscopy uses a thin flexible tube to inspect the ducts and remove stones. ERCP cannot be used to remove stones within your gallbladder.
- Medications: If surgery is not an option, there are medications that can help dissolve gallstones. However, these medications can only be used to dissolve cholesterol stones. The two most common medications are ursodiol (Actigall®) and chenodiol (Chenix®). It may take months or years to dissolve gallstones using medication. Gallstones often recur in these patients within 5 years.
Gallstone Pancreatitis
Pancreatitis is a disease that causes inflammation of your pancreas. Your pancreas is a small organ that helps you digest food by producing enzymes and fluid that break down food. Sometimes a gallstone blocks the pancreatic duct and it causes pancreatitis. When that happens, it’s known as gallstone pancreatitis.
In gallstone pancreatitis, the stone blocks the small opening between the pancreas and the first part of the small intestine (duodenum). This stops the flow of pancreatic enzymes traveling into the small intestine and forces them back into the pancreas. This causes irritation and inflammation of the pancreas known as pancreatitis.
Gallstone pancreatitis can be quite painful and even life-threatening if not treated. Gallstones are the most common cause of acute (short-term) pancreatitis.
Gallstone Pancreatitis Symptoms
The symptoms of gallstone pancreatitis are often similar to gallstone disease. Severe pain is the most common symptom and often occurs suddenly.
- Pain in the upper right or left of your abdomen or in your back
- Pain that radiates to your shoulders or chest
- Nausea, vomiting, and sweating
- Jaundice (yellowing of the skin)
Gallstone Pancreatitis Diagnosis
Diagnosing gallstone pancreatitis uses a combination of tools. Most often this means blood tests and imaging tests. Blood tests can identify inflammation of the pancreas.
Ultrasound, MRI, or CT Scan provide a more accurate picture of the severity of inflammation. These imaging tests can also see if a gallstone is blocking the pancreatic duct which would need to be removed.
Gallstone Pancreatitis Treatment
If pancreatitis is mild, initial treatment involves not eating or drinking until the inflammation improves. This is often done in a hospital setting and IV fluids are given to prevent dehydration. Symptoms usually resolve in a few days.
In more severe cases of inflammation, doctors may treat pain, and nausea, and provide nutrients through an IV. Your doctor will assess whether your gallstone should be removed right away. In some cases, it may be better to wait 24-48 hours for some of the inflammation to subside. Gallstones may pass without further treatment or may require removal through surgery or endoscopy.
If any of the pancreatic tissue becomes infected (pancreatic necrosis), your doctor may recommend antibiotics.
After the pancreas becomes less inflamed, your doctor may recommend the complete removal of your gallbladder. This procedure, known as a cholecystectomy, greatly reduces your chances of having gallstone pancreatitis in the future.
Sphincter of Oddi Dysfunction
What Is Sphincter of Oddi Dysfunction?
The Sphincter of Oddi is a muscle that surrounds the end of the bile and pancreatic ducts. During digestion, this muscle relaxes to allow the flow of bile and pancreatic fluid into the small intestine. With Sphincter of Oddi Dysfunction, this muscle doesn’t open properly, causing digestive fluids to back up. It can cause severe pain and pancreatitis. When fluid backs up into the bile ducts, it’s called biliary dyskinesia.
Sphincter of Oddi Dysfunction is also called post-cholecystectomy syndrome because it’s most common in people who’ve had their gallbladder removed.
Sphincter of Oddi Dysfunction Symptoms
- Abdominal Pain
- Nausea / Vomiting
- Fever / Chills
- Diarrhea
Sphincter of Oddi Dysfunction Diagnosis
Because abdominal pain has many possible reasons, your doctor will check to see if your pain is being caused by another condition. Other, more serious conditions will be ruled out. These could include stones in the bile ducts, pancreatic or bile duct cancer, peptic ulcer disease, or heart disease.
Blood tests may be used to measure liver and pancreatic enzymes.
After other conditions have been ruled out, your doctor may recommend a special type of endoscopy called Oddi manometry. During the procedure, which is done under sedation, a catheter is inserted into the bile and pancreatic ducts. Contrast may be injected and viewed with an x-ray to provide your doctor with images of the ducts. Sphincter of Oddi manometry allows your doctor to see how well the sphincter expands and contracts. If the muscle contracts abnormally (dyskinetic), then biliary dyskinesia is diagnosed.
Sphincter of Oddi Dysfunction Treatment
In mild cases, medications and a low-fat diet are usually the first treatment step. Medications specific to sphincter of Oddi dysfunction don’t exist, but pain and spasms may be reduced with pain medications and antispasmodics.
When the pain is more severe and the doctor has confirmed the diagnosis of sphincter of Oddi dysfunction, more advanced treatments are available. These include botulinum toxin (Botox) injections and sphincterotomy, surgery to cut the muscle.
In a sphincterotomy, the sphincter is cut and cauterized. It should only be attempted by experienced doctors when symptoms do not resolve. Sphincterotomy carries a relatively high complication rate, with 5-15% developing pancreatitis immediately following the procedure.