Patient Education
Gastroparesis
What is Gastroparesis?
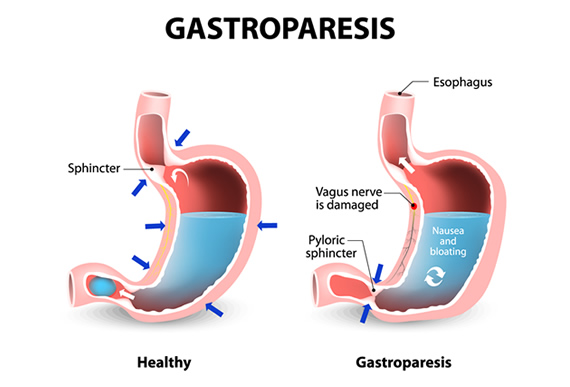
Gastroparesis, also called delayed gastric emptying, is a condition where the stomach is unable to empty food normally. Literally translated, gastroparesis means “stomach paralysis.” Normally, the muscles in the digestive system use contractions to move the food along, but with gastroparesis, damaged muscles and nerves that control the movement can’t function correctly.
It can cause heartburn, nausea, and vomiting, and may be treated with medications or surgery. Gastroparesis is a common condition among people who have had diabetes for a long time but can also occur in people without diabetes.
Gastroparesis Symptoms
It’s possible to have gastroparesis and not have any symptoms. When symptoms are present, they include:
- Heartburn / Acid Reflux / Gastrointestinal Reflux (GERD)
- Nausea
- Vomiting- sometimes undigested food that was eaten hours earlier
- Feeling full quickly when eating
- Abdominal pain or bloating
- Belching
- Loss of appetite / Weight loss / Malnutrition
- Changes in blood sugar
What Causes Gastroparesis?
Gastroparesis can be a complication of surgery or acid reflux, but the underlying cause is often unknown. Diabetic gastroparesis is caused by poorly controlled diabetes. Contrary to what some might think, gastroparesis is not caused by a blockage in the stomach or intestine. In most cases, it is caused by damage to the vagus nerve.
The vagus nerve controls the stomach muscles. If it is damaged, the stomach muscles will not contract and move food out of the stomach and into the small intestine in a normal way. This is also known as delayed gastric emptying.
Potential causes of gastroparesis and vagus nerve damage:
- Diseases, such as diabetes
- Infections
- Abdominal surgery that results in damage to the vagus nerve
Medications Associated with Impaired Gastric Emptying
People with gastroparesis sometimes have problems with certain medications that can slow stomach emptying.
- Narcotics
- Tricyclic antidepressants
- Calcium channel blockers
- Clonidine
|
- Dopamine agonists
- Lithium
- Nicotine
- Progesterone
|
Risk Factors
The risk increases with:
- Diabetes
- Hypothyroidism
- Abdominal or esophageal surgery
- Infection
- Certain medications, including some antidepressants and narcotics.
- Scleroderma (connective tissue condition that can affect internal organs)
- Nervous system disorders, like MS or Parkinson’s.
- Gender: Women are more likely to develop gastroparesis than men.
Gastroparesis Complications
Gastroparesis can severely impact your health, decreasing your overall quality of life. Possible complications include:
- Dehydration – frequent vomiting can lead to severe dehydration, which can become life-threatening.
- Malnutrition- you may not have enough appetite to support your nutritional requirements, or vomiting may prevent you from absorbing enough nutrients.
- Bacterial growth – food that stays in the stomach too long can ferment and lead to bacterial growth.
- Bezoars – bezoars are solid masses that form in the stomach from undigested food. They can cause nausea, vomiting, and could be life-threatening if they block the pathway between the stomach and small intestine.
- Unpredictable blood sugar levels you may not have enough appetite to support your nutritional requirements, or vomiting may prevent you from absorbing enough nutrients.
Diagnosis
Gastroparesis is often misdiagnosed because other conditions like heartburn may have similar symptoms. There are several tests used to determine if you have gastroparesis. In addition to reviewing your medical history, performing a physical exam, and blood tests, your doctor may recommend the following tests or procedures to aid in diagnosis:
Upper Endoscopy
Using a thin, lighted tube with a camera on the end, the doctor will inspect the esophagus, stomach, and the first part of the small intestine. This test may also rule out other conditions that have the same symptoms as gastroparesis.
Gastric Emptying Study
One of the most definitive tests in diagnosing gastroparesis is a gastric emptying study. In this test, patients eat a small meal (such as an egg or oatmeal) with a small amount of radioactive material. Then, a scanning device is used to track the progress of food through the stomach. Talk to your doctor about any medications you’re taking before this study, as some could impact the results.
SmartPill
The SmartPill is a small, non-digestible wireless capsule that transmits information about digestion to a receiver the patient wears around their waist. The information includes the pH level, temperature, and pressure changes throughout the digestive tract. This can help determine how quickly the stomach is emptying.
Imaging Tests
Your doctor may recommend an ultrasound or upper GI series x-ray to rule out other possible causes of your symptoms.
Gastroparesis Treatment & Diet
There is no cure for gastroparesis, but medication and diet changes can help in most cases. In very severe cases, surgery may be recommended.
Treatment usually begins by identifying and treating the underlying cause of gastroparesis. If the cause is diabetes, your doctor will make recommendations for treatment.
Gastroparesis Diet
Making sure you get adequate nutrition is important when managing gastroparesis. Diet changes usually help people manage gastroparesis and are the first step in treatment. It may be helpful to visit with a registered dietitian who can work with you to identify foods that are easier to digest.
Most people can lead a relatively normal life by eating softer foods and drinking supplemental nutritional drinks to ensure they get the calories and nutrients they need.
Other gastroparesis diet advice includes:
- Eat smaller meals (instead of 3 meals a day, have 5 or 6 smaller meals throughout the day)
- Chew food completely
- Choose cooked vegetables and fruits over raw, uncooked fruits and vegetables
- Avoid high-fiber vegetables and fruits, like broccoli and oranges
- Avoid fatty foods (these can slow digestion)
- Puree your food or eat soups if liquids are easiest to swallow
- Drink plenty of water each day (1 to 1.5 liters)
- Take a walk after you eat
- Avoid alcohol, smoking, and carbonated beverages
- Try not to lay down within 2 hours of eating
- Take a daily multivitamin
Below are recommended diet choices for people with gastroparesis. This is not an exhaustive list, and a dietitian can provide a more complete list.
Starches
- White bread and rolls
- Light-colored whole wheat bread (without seeds or nuts)
- Plain bagels
- English muffins
- Corn and flour tortillas
- Pancakes
- Cream of wheat
- Saltines and other white crackers
- White potatoes and sweet potatoes (without skin)
- French fries (baked only, not fried)
- Rice
- Pasta
|
Proteins
- Lean beef, pork, and veal
- Chicken and turkey (not fried and without skin)
- Lobster, crab, shrimp, oysters, clams, scallops
- Tuna (in water, not oil)
- Cottage cheese
- Tofu
- Eggs
|
Fruits and vegetables
- Tomato sauce, puree, paste, juice
- Cooked carrots, beets, and mushrooms
- Vegetable broth and juice
- Fruit drinks and juices
- Applesauce
- Bananas
- Pears and Peaches (canned)
|
Dairy
- Milk (if tolerated)
- Yogurt
- Pudding and custard
- Frozen Yogurt
|
Gastroparesis Medications
Medications typically fall into two categories: those that stimulate muscles to move food through the gastrointestinal tract and those that control nausea and vomiting:
- Metoclopramide (Reglan) – This medication acts on the dopamine receptors in the stomach and can stimulate the stomach muscles. It is also used to reduce nausea and vomiting. Serious side effects can occur, and it should not be taken long term.
- Ondansetron (Zofran) and prochlorperazine (Compazine) – These both help stop nausea and vomiting.
- Erythromycin (Eryc, E.E.S.) – erythromycin is an antibiotic that stimulates the motilin receptors of the stomach. This causes the stomach to contract and pass food. Over time, a medication tolerance can build up making the medication less effective with long-term use. This medication may also cause diarrhea.
- Domperidone – This medication also acts on the dopamine receptors, but has shown to have fewer side effects than Metoclopramide. Its use is restricted in the United States but domperidone is used in Mexico, Canada, and European countries. The FDA has restricted its use in the United States due to concerns about serious side effects. However, there may be certain circumstances where its use is approved.
Gastroparesis Surgery
Surgery for gastroparesis is reserved for people with severe symptoms that do not respond to other treatments. Surgical options include the placement of venting tubes into the stomach. These venting tubes may reduce symptoms in patients with recurrent dehydration and vomiting.
Feeding tubes can be used in those who can’t tolerate any food or liquid. A feeding tube called a percutaneous jejunostomy can be inserted surgically into the small intestine, or a temporary feeding tube can be inserted through the nose or mouth.
In some cases, the lower part of the stomach may be stapled or bypassed to improve stomach emptying.
Electrical Stimulation for Gastroparesis
One area of medical research is looking at electrical stimulation to treat gastroparesis. Small electronics are attached to the stomach wall. Once activated, they can cause the stomach to contract. Studies haven’t shown significant improvements in stomach emptying, but have shown to reduce bothersome symptoms like nausea and vomiting.
Diabetic Gastroparesis
The most common cause of gastroparesis is diabetes. It’s especially concerning for people with diabetes, as it can destabilize blood sugars. This condition affects how quickly the body digests food and how quickly it absorbs nutrients, making it difficult to dose insulin correctly. It also causes frequent vomiting, which can lead to dangerous dehydration.
You may be able to control symptoms by eating six small meals per day instead of three larger meals. Your doctor may also want you to adjust your insulin dosing.
The best way to prevent diabetic gastroparesis is to manage your diabetes, keeping your blood sugar close to your target range.
FAQ
What foods should you avoid if you have gastroparesis?
Foods to avoid with gastroparesis include raw fruits and vegetables, fibrous fruits and vegetables (oranges, broccoli), high-fat foods, carbonated drinks, and alcohol.
What is the best treatment for gastroparesis?
The best treatment for gastroparesis will depend on each individual patient and their response to treatment. Medications and surgery should only be considered after dietary and lifestyle changes.
Can you reverse gastroparesis?
There is no cure for gastroparesis, but most people can find relief through dietary changes and medication.
Are bananas good for gastroparesis?
Yes, bananas are considered ‘safe’ food for people with gastroparesis.
Can gastroparesis kill you?
Gastroparesis is generally non-life-threatening, but the complications can be serious. They include malnutrition, dehydration, or a bezoar completely blocking the flow of food out of the stomach.
What causes gastroparesis?
Diabetes is the most common cause of gastroparesis, but it may also be caused by nerve injury, especially to the vagus nerve. Other possible causes are abdominal surgery, amyloidosis, medications, scleroderma, and viral infections. The cause is often unknown.
What is gastroparesis life expectancy?
When gastroparesis is managed well, it does not affect life expectancy. However, several conditions that cause gastroparesis like MS, Parkinson’s disease, or diabetes, can have other complications that lead to a decreased life expectancy.