Patient Education
Liver Cirrhosis
What is Cirrhosis?
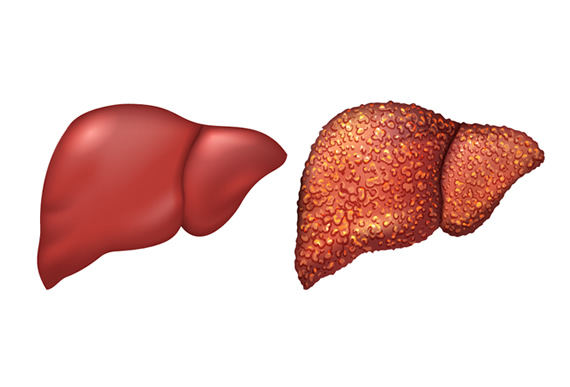
Cirrhosis is a liver condition in which healthy tissue is replaced by scar tissue. The scar tissue forms when the liver tries to repair itself after injury. Common causes of liver injury include chronic alcoholism, hepatitis, and other medical conditions.
As scar tissue replaces more and more healthy tissue over time, it can affect the liver’s ability to function properly. Extensive liver damage could be life-threatening.
Cirrhosis Symptoms
Most patients with cirrhosis won’t have symptoms until liver damage is significant. When that happens, the symptoms can include:
- Loss of appetite
- Fatigue / Lack of energy
- Bruises
- Itchy skin
- Weight loss
- Jaundice (Yellow discoloration of the skin/eyes)
You should see a doctor if you have any of these symptoms. Schedule an appointment.
Cirrhosis Causes
There are many different conditions and diseases that can cause cirrhosis.
The most common cirrhosis causes are:
- Viral Infections – including hepatitis B and C
- Alcohol abuse
- Fatty liver
Other cirrhosis causes include:
- Hemochromatosis (buildup of iron in the body)
- Cystic Fibrosis
- Wilson’s Disease (abnormal storage of copper in the liver)
- Bile duct blockage
- Alpha-1 antitrypsin deficiency
- Inherited disorders
- Drug-induced injury
- Autoimmune diseases
Cirrhosis Risk Factors
- Excessive alcohol consumption – Those who drink too much alcohol have an increased risk of developing cirrhosis
- Obesity – Being overweight increases your chances of developing a condition that can lead to cirrhosis like fatty liver disease.
- Viral hepatitis infection – Patients with chronic hepatitis are at a higher risk of developing cirrhosis.
Cirrhosis Diagnosis
Early-stage cirrhosis usually doesn’t cause symptoms, but may cause abnormalities during routine blood work and checkups. To confirm the diagnosis of cirrhosis, doctors may perform:
- Physical Exam – Your doctor can observe the size and texture of the liver. Healthy livers are smooth, and cirrhotic livers are irregular and bumpy.
- Blood Tests – Your doctor may perform blood tests to check for liver conditions.
- Imaging tests – Ultrasound, CT, or MRI may be used to take pictures of the liver
- Biopsy – Your doctor may perform a liver biopsy. A small tissue sample is removed from the liver and examined.
Cirrhosis Treatment
Treatment for cirrhosis falls into two categories: Treating the underlying cause of cirrhosis and treating the complications/symptoms of cirrhosis.
Treatment for the causes of cirrhosis:
- Stop Drinking – Those with cirrhosis caused by excessive alcohol use should seek treatment for alcohol dependency. Stopping alcohol use can be difficult, and your doctor may have treatment recommendations. Alcohol is toxic to the liver, so it is critical for patients with cirrhosis to stop drinking.
- Lose Weight – Those with cirrhosis caused by nonalcoholic fatty liver disease may slow the progression of cirrhosis by losing weight.
- Treatment for hepatitis – Taking medication to control viral infections like hepatitis can limit further damage to the liver.
Treatment for the symptoms/complications of cirrhosis:
- Symptoms – Treatment for cirrhosis symptoms like fatigue, itching, and pain may be prescribed.
- Fluid retention – Edema (fluid retention) is treated by reducing salt in the diet. Diuretic medications (water pills) to reduce excess water may also be prescribed.
- Infections – Your doctor may recommend antibiotics or other treatments for infections.
- Vaccinations – Your doctor will likely recommend vaccinations for influenza, pneumonia, and hepatitis.
- Hepatic Encephalopathy – This condition can cause confused thinking in patients who have had cirrhosis for a long time. The liver’s ability to remove toxins is reduced in patients with cirrhosis. When those toxins enter the bloodstream, it can cause a decline in brain function.
- Liver cancer – the chance of liver cancer is increased with cirrhosis. Your doctor may recommend periodic blood and imaging tests to look for cancer.
- Varices – Abnormally enlarged veins called varices may occur in patients with cirrhosis. Most often, varices are found in the esophagus. Your doctor may recommend an upper-endoscopy to look for varices.
- Ascites – Abnormal amount of fluid found inside the abdominal cavity. In mild cases, it may only be observed through imaging tests like an ultrasound or CT scan. If ascites becomes infected, it’s called Bacterial Peritonitis.
Liver Transplant
In advanced cases when the liver is failing, a liver transplant may be the only treatment option. In this surgery, your liver is replaced with a healthy liver from a deceased donor. In some cases, part of a healthy liver may be donated by a living donor.
Transplant surgery is a major undertaking and requires lifelong anti-rejection medication. Extensive testing is required to ensure a candidate is healthy enough for a transplant.
Cirrhosis FAQ
What does the liver do?
The liver serves many important functions vital to life, including:
- Processes the blood from the digestive system before it’s sent back to the heart.
- Extracting nutrients from the blood
- Making bile – which helps the digestive system absorb vitamins and fat
- Removing medications and toxins from the blood
- Producing blood proteins, including the ones responsible for normal blood clotting.
How many people have cirrhosis?
Around 5.5 million people in the United States are affected by cirrhosis. That’s roughly 2% of the US population. Cirrhosis can be attributed to 26,000 deaths each year, and that number is expected to rise.
Liver Cirrhosis Testimonial
“I began to see Dr. Ali right after the pandemic started. He was able to diagnose and treat me for my fatty almost cirrhosis liver. With his help, my liver levels dropped 75% and my liver is now functioning normally. My IBS has also been controlled with his help. Thank you, Dr. Ali!” -Brianna