Patient Education
Pancreatitis
What is Pancreatitis?
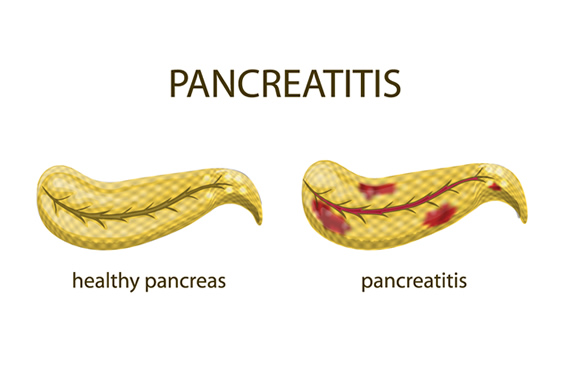
Inflammation of the pancreas is called pancreatitis. The pancreas is a gland near the stomach and the duodenum (upper part of small intestine). It serves two primary purposes:
- Produce enzymes that help digestion
- Produce hormones, like insulin and glucagon, that help regulate the sugar (glucose) in the bloodstream.
Digestive enzymes from the pancreas normally do not become active before reaching the small intestine. However, if the pancreas is inflamed, the enzymes can activate within the pancreas and cause tissue damage.
Treatment may not be necessary for mild pancreatitis, but severe pancreatitis can cause life-threatening complications.
Acute and Chronic Pancreatitis
There are two types of pancreatitis.
- Acute pancreatitis is when the condition appears suddenly and lasts for days. Depending on the severity, acute pancreatitis can be life-threatening. Gallstones and heavy alcohol use are common causes. Acute pancreatitis may occur within hours or as long as two days after consuming alcohol.
- Chronic pancreatitis is when the condition occurs over several years, and does not heal or improve. It develops most often in people between the ages of 30 and 40 and is often linked to years of heavy alcohol use.
It can be triggered by a single acute attack that causes damage to the pancreatic duct. That damage causes inflammation and scar tissue, which slowly destroys the pancreas.
Symptoms
The signs of pancreatitis may vary between acute and chronic cases.
Acute pancreatitis symptoms include:
- Pain in the upper abdomen
- Abdominal pain that radiates to your back
- Swollen or tender abdomen
- Nausea / Vomiting
- Rapid pulse
- Fever
Chronic pancreatitis symptoms include:
- Pain in the upper abdomen
- Pain in the abdomen that is worse after eating
- Weight loss (unintentional)
- Nausea / Vomiting
- Diarrhea
- Oily stools
Schedule an appointment if you have persistent abdominal pain. If you have severe abdominal pain, seek immediate care.
Causes
Acute Pancreatitis Causes
The most common acute pancreatitis cause is gallstones. Gallstones are stone-like formations that develop in the gallbladder. As gallstones pass through the common bile duct, they can cause inflammation of the pancreas. Heavy alcohol use is also common. Possible acute pancreatitis causes include:
- Gallstones
- Heavy alcohol use
- Trauma or Surgery in to the abdomen
- Infections
- Medications
- Tumors
- Genetic abnormalities
- Hypertriglyceridemia (high levels of triglycerides, a type of blood fat)
- Hypercalcemia (high levels of calcium in the blood)
- Pancreatic cancer
- Cystic fibrosis
- Obesity
Chronic Pancreatitis Causes
- Hereditary disorders of the pancreas
- Cystic fibrosis (the most common inherited disorder)
- Hypercalcemia (high levels of calcium in the blood)
- Hyperlipidemia or hypertriglyceridemia (high levels of blood fats)
- Certain medications
- Certain autoimmune conditions
- Long-term alcohol use
- Unknown causes
Hereditary pancreatitis may be present in someone under 30 years old but may go undiagnosed for several years. Brief periods of abdominal pain and diarrhea may come and go and eventually lead to chronic pancreatitis.
This is more common in people who have two or more family members that have pancreatitis across more than one generation.
Risk Factors for Pancreatitis
There are no factors that guarantee you’ll develop pancreatitis, but certain factors increase your risk, like:
- A family history of pancreatitis
- A personal or family history of gallstones
- Cystic fibrosis
- Diabetes
- Elevated triglycerides
- Gender – men have a higher risk
- Genetic issues of the pancreas
- Heavy alcohol use
- Obesity
- Race – African Americans have a higher risk
- Smoking cigarettes
- Some autoimmune conditions
Diagnosing Pancreatitis
Doctors will review a person’s medical history, perform a physical examination, and order blood tests to diagnose pancreatitis. During cases of acute pancreatitis, the blood will have high levels of the digestive enzymes formed in the pancreas.
Procedures and tests used to diagnose pancreatitis include:
- Blood tests – These tests check the levels of liver and pancreatic enzymes, signs of inflammation or infection, levels of blood sugar and lipids (blood fats), and look for signs of pancreatic cancer.
- Urine or Stool Tests (for chronic pancreatitis)- A test can measure the amount of fat in the stool to determine how well the digestive system absorbs nutrients. Urine tests can measure the amount of an enzyme called amylase, which may indicate a problem with the pancreas.
- CT Scan – A type of x-ray that can create 3-D images of internal organs, a CT scan lets your doctor identify gallstones and pancreatic inflammation.
- Ultrasound – Another type of imaging that uses sound waves to visualize internal organs, an ultrasound may show gallstones and inflammation.
- Endoscopic Ultrasound (EUS) – A combination of technology, using an endoscope and ultrasound. The endoscope is a thin, lighted tube that is inserted through the mouth and down into the digestive tract. The endoscope is fitted with an ultrasound attachment that produces images of the bile and pancreatic ducts so your doctor can look for blockages or inflammation.
- MRI – Magnetic resonance imaging can be used to look for signs of inflammation or damage in the pancreas or other causes of pancreatitis in the bile ducts and gallbladder.
Treatment of Pancreatitis
Treatment for pancreatitis may involve hospitalization. Treatments may include:
- Nutrition – If you can’t tolerate food, you may get nutrition through an IV or a feeding tube until you can tolerate food again. Clear liquids and bland foods can be reintroduced once the inflammation is controlled, followed by a low-fat diet. Eventually, you can resume a normal diet. If inflammation persists, a feeding tube may be recommended for proper nutrition.
- Medications for Pain – Severe pain is common with pancreatitis. There are medications that can help.
- IV Fluids – Intravenous fluids will be provided during a hospital stay to ensure proper hydration and nutrient levels.
The underlying cause of pancreatitis will be treated separately once inflammation is under control. Treatment will depend on the underlying cause, and may include:
- Removing obstructions in the bile duct – If pancreatitis is caused by a blocked or narrowed bile duct, it could require a procedure to restore normal function.
- Endoscopic Retrograde Cholangiopancreatography (ERCP) is a procedure that uses a thin tube with a small camera to examine the bile ducts and pancreas. This procedure can help diagnose problems. It also carries a slight risk of complications including severe pancreatitis, bowel perforation, infection, or bleeding. Some procedures are performed using ERCP include
- Sphincterotomy – In this procedure, a tiny incision is made in the muscle surrounding the pancreatic or bile duct using a small wire on the endoscope. This helps enlarge the duct opening.
- Gallstone removal – If gallstones are present, a small basket on the endoscope may be used to retrieve pancreatic or bile duct stones.
- Stent placement – A small piece of plastic or metal resembling a small straw can be inserted into the bile or pancreatic duct to keep it open.
- Balloon dilation – Some endoscopes can inflate a small balloon to dilate (stretch) the bile or pancreatic duct. A stent may be used temporarily.
- Gallbladder surgery – If pancreatitis is caused by gallstones, surgery to remove your gallbladder (cholecystectomy) may be recommended.
- Pancreas surgery – If fluid needs to be drained from the pancreas, or diseased tissue needs to be removed, it may require surgery.
- Alcohol treatment – If alcohol dependence is the cause of pancreatitis, your doctor may recommend treatment for alcohol addiction. Drinking could worsen pancreatitis and cause serious complications.
- Medication change – If the medication was the cause, other options may be prescribed.
- Synthetic pancreatic enzymes – If the pancreas doesn’t make enough enzymes on its own, the doctor may prescribe additional enzymes to be taken with meals to help process nutrients.
- Dietary changes – A nutritious, low-fat diet is important for people with pancreatitis. A registered dietitian can help develop a meal plan. Drinking plenty of fluids, avoiding caffeine, and eating more numerous, smaller meals daily instead of fewer large ones will also help manage pancreatitis.
Complications of Pancreatitis
Pancreatitis can cause some complications, including:
- Pseudocysts – Cyst-like pockets in the pancreas that collect fluid and debris. If a pseudocyst ruptures, it could cause further complications like infection and internal bleeding.
- Infection – Pancreatitis can make the pancreas vulnerable to infection, a serious complication that can require surgery.
- Kidney failure – Dialysis may be necessary to treat kidney failure caused by pancreatitis.
- Breathing problems – In rare cases, pancreatitis can cause chemical changes in your body, leading to breathing problems that keep you from getting enough oxygen in your blood.
- Malnutrition – Pancreatitis can cause lower levels of the enzymes needed to break down food and process nutrients. This can cause malnutrition, weight loss, and diarrhea.
- Diabetes – If the insulin-producing cells of the pancreas are damaged, diabetes may develop.
- Pancreatic cancer – The inflammation from chronic pancreatitis increases the risk of developing pancreatic cancer.
- Dehydration – Vomiting, diarrhea, and outside factors like warm temperatures can quickly lead to dehydration with pancreatitis. Severe dehydration can lead to serious or life-threatening complications.
FAQ
Where is the pancreas?
The pancreas is located in the upper abdomen near the stomach and the first part of the small intestine (duodenum).
What is the most common cause of pancreatitis?
Some of the most common causes of pancreatitis include gallstones and heavy alcohol use.
How dangerous is pancreatitis?
Pancreatitis can be dangerous if it goes undiagnosed and untreated. If you have symptoms, you should seek medical attention.
How can I treat pancreatitis at home?
Pancreatitis shouldn’t be treated at home, but you can take steps to aid the healing process and help reduce or prevent symptoms from recurring:
- Stop drinking alcohol
- Stop smoking
- Eat a low-fat diet
- Stay hydrated (drink more fluids)