Patient Education
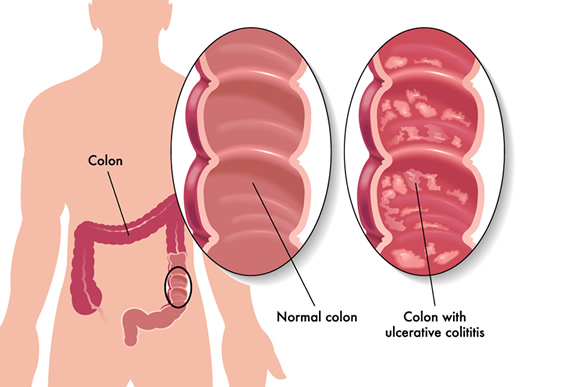
Ulcerative Colitis
What is Ulcerative Colitis?
Ulcerative colitis (UC) is a long-lasting inflammatory bowel disease (IBD) that causes inflammation and ulcers in the large intestine. The large intestine includes the rectum and colon. In patients with UC, the immune system mistakenly targets the lining of the large intestine. This can cause inflammation, ulceration, bleeding, and diarrhea in the colon and rectum.
There is no cure for ulcerative colitis, but treatment can usually control and reduce the symptoms. Most people with ulcerative colitis live productive and active lives.
Symptoms
In most people, the symptoms of ulcerative colitis develop slowly over time, but it can also start suddenly. Symptoms of ulcerative colitis will vary based on where inflammation occurs and how severe it is. Symptoms can be mild to severe and include:
- Anemia
- Fatigue
- Diarrhea – may include blood or pus
- Abdominal pain/cramping
- Rectal pain/bleeding
- Straining to defecate / constipation
- An urgent need to defecate
- Fever
- Dehydration
- Loss of appetite, weight Loss
The symptoms of ulcerative colitis may come and go. When symptoms are active, it’s called a flare. Symptom-free periods between flares are called remission. A remission period can last for years, but symptoms will eventually return. Each person’s experience with ulcerative colitis is different, making it difficult to predict flares or remission.
Causes and Risk Factors
Research hasn’t found the cause of ulcerative colitis but does show that it is more common in people with certain risk factors, including:
- Genetics – Ulcerative Colitis often runs in families, which suggests a genetic role.
- Environment – Infections can trigger an abnormal immune response in those susceptible to UC.
- Immune System – If triggered, the immune system targets the large intestine and causes inflammation.
- Geographic location – Ulcerative Colitis appears to be more common in those living in northern climates and developed countries (North America, Great Britain) compared to those living in developing countries and southern climates. Doctors do not yet know the reasons for these correlations.
- Age: UC can occur at any age, but often begins before age 30. Some may not develop UC until after age 60.
- Race / Ethnicity: Although white people have the highest risk, UC can occur in all races. The risk for those of Ashkenazi Jewish descent is even higher.
- Family history: If a close relative like a parent, sibling, or child has UC, you have a higher risk.
Men and women are at equal risk for ulcerative colitis.
Types of Ulcerative Colitis
There are four types of ulcerative colitis. The type is determined by the location of the disease; however, symptoms of each are often similar.
There are several types of ulcerative colitis, including:
- Ulcerative proctitis – When the disease is limited to the rectum, it’s called ulcerative proctitis. Sometimes, the only symptom is rectal bleeding.
- Distal colitis/proctosigmoiditis – When the inflamed area extends into the lower part of the colon, the mid-sigmoid colon, it’s called distal colitis or proctosigmoiditis. Symptoms may include abdominal pain and cramping, bloody diarrhea, and an urge to have a bowel movement without success (tenesmus).
- Left-sided colitis – When inflammation extends to (but not beyond) the splenic flexure. The splenic flexure is the sharp turn in the intestines where the transverse colon meets the descending colon. Symptoms can include bloody diarrhea, left-sided abdominal pain and cramping, an urgent need to defecate, and weight loss.
- Extensive colitis/pancolitis – When inflammation spans the entire colon, from the rectum to past the splenic flexure, but not into the cecum (where the colon begins). Symptoms can include abdominal pain, bloody diarrhea, loss of appetite, and weight loss.
Ulcerative Colitis Complications
Ulcerative colitis itself is often not fatal, but it can cause complications. Some can be serious or even life-threatening. Complications include:
- Anemia
- Severe rectal bleeding
- Perforated colon (a hole in the colon)
- Severe dehydration
- Osteoporosis (bone loss)
- Inflammation of the eyes, skin, joints, liver, and bile ducts
- Higher risk of colon cancer
- Toxic megacolon (a rapidly swelling colon)
- Fulminant ulcerative colitis, a severe form of UC
- Higher risk of blood clots in the arteries and veins
Diagnosis
The doctor will diagnose ulcerative colitis after ruling out other causes of signs and symptoms. To confirm the diagnosis of ulcerative colitis, your doctor may recommend the following tests and procedures:
- Blood tests: Blood tests can check for anemia and signs of an infection. Anemia is a condition when the blood doesn’t have enough healthy red blood cells.
- Stool tests: Stool tests look for white blood cells that could indicate ulcerative colitis. These tests can also rule out other conditions like infections caused by parasites, viruses, or bacteria.
- Colonoscopy: This exam allows the doctor to view the inside of the colon using a thin, lighted tube with a camera. A colonoscopy also allows the doctor to remove small tissue samples (biopsies) that can be tested to confirm a diagnosis of UC.
- Flexible sigmoidoscopy: If the colon is severely inflamed, the doctor may recommend a sigmoidoscopy instead of a colonoscopy. A sigmoidoscopy exam allows the doctor to view the last portion of the colon, including the rectum and sigmoid.
- X-ray: The doctor may recommend a traditional abdominal X-ray if you have severe symptoms. This helps rule out more serious conditions like a perforated colon.
- CT Scan – If complications from UC are suspected, the doctor may recommend an abdominal CT scan. This imaging scan may also determine the severity and location of the inflammation.
Ulcerative Colitis Treatment
Since ulcerative colitis is a chronic disease, it requires ongoing treatment. When treatment is successful, it keeps you in remission (without symptoms) long-term. Treatment for UC usually involves medications or surgery.
The type of medication your doctor recommends will depend on the severity of the condition. Some drugs work better than others for certain people. It may take time to determine the best medication for your symptoms.
Your doctor will work with you to find a medication that works best for you. Some medications have side effects, which each patient will need to consider when deciding how to treat their ulcerative colitis.
Medications
Anti-inflammatory Drugs
The first step in treating ulcerative colitis is usually anti-inflammatory drugs.
- 5-aminosalicylates – Sulfasalazine (Azulfidine), mesalamine (Asacol HD, Delzicol, others), balsalazide (Colazal), and olsalazine (Dipentum), and other antibiotics may be used when an infection occurs. Doctors may also prescribe them to treat complications of ulcerative colitis. Your doctor will help you determine the best drug based on your condition.
- Corticosteroids (steroids) – These drugs, including prednisone and hydrocortisone, reduce inflammation by suppressing the immune system. They are usually recommended for moderate or severe ulcerative colitis that isn’t responding to other treatments. They are not usually given long-term due to potential side effects.
Immune system modifiers
Immunosuppressant drugs reduce inflammation by suppressing the immune system response that causes inflammation. A combination of these medications may be more effective for some people.
- Azathioprine (Azasan, Imuran) and mercaptopurine (Purinethol, Purixan). These immunosuppressants are frequently used with other medications, called biologics. While taking them, it’s important to have your blood checked regularly to look for side effects (including pancreas and liver problems).
- Cyclosporine (Gengraf, Sandimmune, and Neoral). This is usually a last-resort medication when other medications haven’t helped. Cyclosporine can cause serious side effects and is not intended for long-term use.
- Infliximab (Remicade), adalimumab (Humira) and golimumab (Simponi). These drugs are biologic therapies (biologics) that suppress the immune system by targeting a specific pathway, reducing inflammation. They are usually given to people with severe ulcerative colitis and those who don’t respond to or can’t tolerate conventional therapy.
- Vedolizumab (Entyvio). This medication blocks inflammatory cells from the site of inflammation. It’s reserved for those who don’t respond to or can’t tolerate conventional therapy.
- Ustekinumab (Stelara). This medication blocks a specific protein to prevent inflammation. It’s also used when other treatments don’t work or aren’t well tolerated.
Other medications
Other medications may be necessary to treat the symptoms of ulcerative colitis, including:
- Antibiotics – Metronidazole, ciprofloxacin, or other antibiotics may be used during an infection, or to treat ulcerative colitis complications.
- Anti-diarrheal medications – Anti-diarrheal medications should only be used after talking with your doctor since they can increase the risk of toxic megacolon. Loperamide (Imodium) may be effective for treating severe diarrhea.
- Pain relievers. The doctor may recommend acetaminophen (Tylenol) for mild pain. Doctors don’t recommend Ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve), and diclofenac sodium (Voltaren). These drugs can worsen your symptoms and the severity of your condition.
- Iron supplements. Your doctor may recommend taking iron supplements if you have chronic intestinal bleeding that results in iron deficiency anemia.
Ulcerative Colitis Surgery
Surgery has the benefit of eliminating ulcerative colitis. However, it’s only considered if other treatments like medications haven’t worked. Ulcerative colitis surgery usually means removing the colon and rectum (proctocolectomy). Ileoanal anastomosis surgery (J-pouch) removes the affected part of the colon but still allows the patient to defecate normally after surgery. When that’s not possible, stool must be passed through a stoma in the abdomen into an external pouch.
Psychological Therapy
Because stress can make ulcerative colitis worse, counseling or psychotherapy may be recommended. This can help people with UC who experience frustration, anxiety, or depression.
Cancer Screenings
Due to the increased risk for colon cancer, treatment for UC includes more-frequent cancer screenings. The frequency will depend on how long you’ve had the condition and its severity. When inflammation is confined to the rectum, additional screening isn’t necessary. Otherwise, you may need a colonoscopy every year or two beginning several years after diagnosis.
Diet
There is no firm evidence that diet causes ulcerative colitis, but people may experience worsening symptoms when they eat certain foods. Not everyone will react to different foods in the same way. Keeping a food diary can help you determine which foods aggravate your symptoms.
Some ulcerative colitis diet recommendations include:
- Limit dairy products – Often, those with inflammatory bowel diseases find that limiting or eliminating certain dairy products can improve symptoms like diarrhea and abdominal pain.
- Limit fiber – Some high-fiber foods, like whole grains and fresh fruit and vegetables, may make symptoms worse. Other problem foods may include foods in the cabbage family, broccoli, cauliflower, nuts, seeds, corn, and popcorn. Talk with your doctor or a dietitian to make sure you’re getting enough fiber.
- Drink plenty of fluids daily. Avoid alcohol, caffeine, and carbonated drinks.
- Avoid spicy foods that may make symptoms worse.
- Smaller meals may be more tolerable. Instead of eating two or three large meals per day, try eating five or six smaller meals.
Stress Reduction
Stress doesn’t cause ulcerative colitis, but stress can make symptoms worse. Some ways to control stress include:
- Exercise
- Mindfulness
- Meditation
- Breathing Exercises
- Yoga
Alternative Medicine / Treatments
It’s important to discuss any alternative medicines you may be taking with your doctor, as some may negatively impact your body’s response to traditional therapies.
- Herbal supplements – Most alternative therapies and supplements are not regulated by the FDA, which means they may not be safe or effective.
- Probiotics – Research is limited and results have not been proved, but researchers suspect that adding more good bacteria (probiotics) to the digestive tract may have a positive effect in people with ulcerative colitis.
Testimonial
“I love Dr. Jackson and Nancie sooooo much! I have been receiving treatment from Dr. Jackson since the summer of 2017. He was the one to diagnose me with UC and I’ll never forget the urgency and concern he had in his face and voice when he looked over at my mom and me. He told us that I needed a colonoscopy immediately because I looked very ill and he squeezed me into his busy schedule. I can’t ever imagine switching Doctors. I have always felt taken care of, comfortable and safe when speaking to Dr. Jackson and his nurse Nancie. Being diagnosed with severe Ulcerative Colitis has been the worst thing to happen to me and it really takes a toll on you mentally, physically, and emotionally, but knowing I have an amazing Dr and nurse by my side makes it a lot easier to deal with. I’m happy to say I’m recently diagnosed with mild Ulcerative Colitis and although I’d like it to stay that way, I know this disease is unpredictable but I feel comfort in knowing I have an amazing medical team there for me when I need them. Thank you so much for all the care and support you have shown me over the years. I truly appreciate y’all!” -Brandie